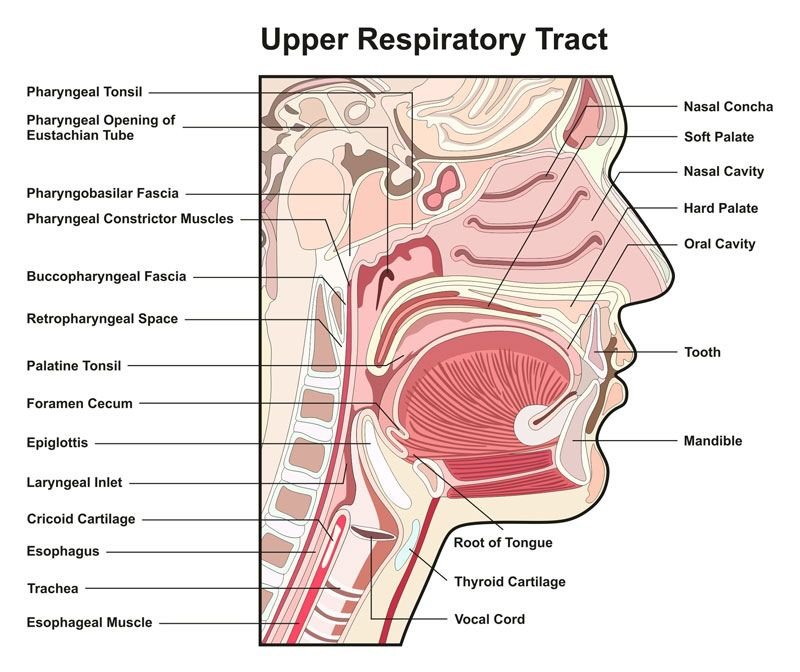
Upper respiratory tract infections (URTIs) emerge from acute assaults targeting the upper respiratory system, encompassing the nasal passages, sinuses, throat, larynx, and trachea. These ailments manifest through a spectrum of symptoms, such as nasal congestion, throat soreness, tonsil inflammation, pharynx irritation, larynx inflammation, sinus inflammation, middle ear inflammation, and the familiar common cold. While predominantly viral, URTIs can also stem from bacterial, fungal, or helminthic sources, albeit less frequently. Indications of URTIs comprise throat discomfort, runny nose, nasal blockage, head pain, mild fever, facial tension, and bouts of sneezing. Notably, antibiotics have no efficacy against viral URTIs, being solely effective against bacterial adversaries. Typically, URTIs subside autonomously within 1 to 2 weeks, with management focused on rest, hydration, and alleviating symptoms through analgesics.
Common causes of upper respiratory tract infections
Upper respiratory tract infections (URTIs) typically stem from viruses, although bacteria, fungi, or helminths can also be implicated, albeit less frequently. Viruses, notably, take the lead in URTIs, resulting in afflictions like the common cold, influenza, coughing spells, and viral pharyngitis. Bacterial agents like Streptococcus pneumoniae are additional contributors to URTIs, including pneumonia. It’s noteworthy that while viruses are the principal instigators of URTIs, bacterial infections can also play a role in exacerbating these respiratory ailments.
Read also: URINARY TRACT INFECTIONS: DECODING HIDDEN RISKS & PREVENTION
Types of upper respiratory tract infections
Types of upper respiratory tract infections (URTIs) include various conditions affecting different parts of the upper respiratory system. Common types of URTIs are:
Rhinitis
Rhinitis presents as inflammation or malfunction of the nasal cavity lining, manifesting symptoms such as nasal congestion, sneezing, and postnasal drip. Its classifications include Allergic Rhinitis (AR), Infectious Rhinitis, and Non-Allergic, Non-Infectious Rhinitis (NAR).
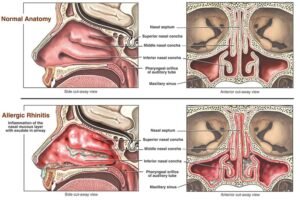
Allergic Rhinitis
Allergic rhinitis stems from allergen triggers, provoking immune responses involving IgE antibodies and histamine release. Pollen or mold spores typically cause seasonal allergic rhinitis (commonly known as “hay fever”), while pet dander, dust mites, or mold can spark perennial allergic rhinitis.
Non-Allergic Rhinitis
Non-allergenic Rhinitis,
In contrast, diverse non-allergen stimuli such as air irritants, weather fluctuations, infections, medications, and odors instigate it. Its precise cause remains elusive, although it implicates nasal blood vessel dilation, inducing congestion, mucus production, and swelling. This form of rhinitis may persist long-term, emerging predominantly after the age of 20, with triggers varying among individuals.
Idiopathic Rhinitis
Rhinitis may also manifest as idiopathic, lacking clear causation, and primarily diagnosed through clinical assessment based on symptoms and medical history.
Management and Treatment
Treatment modalities for rhinitis encompass air humidification, antihistamines, topical anticholinergics, desensitization immunotherapy, nasal corticosteroids, oral decongestants, and saline irrigation. Effective management involves evading triggers like specific foods, irritants, smoke, and allergens while upholding a clean environment to minimize exposure to dust and other particles.
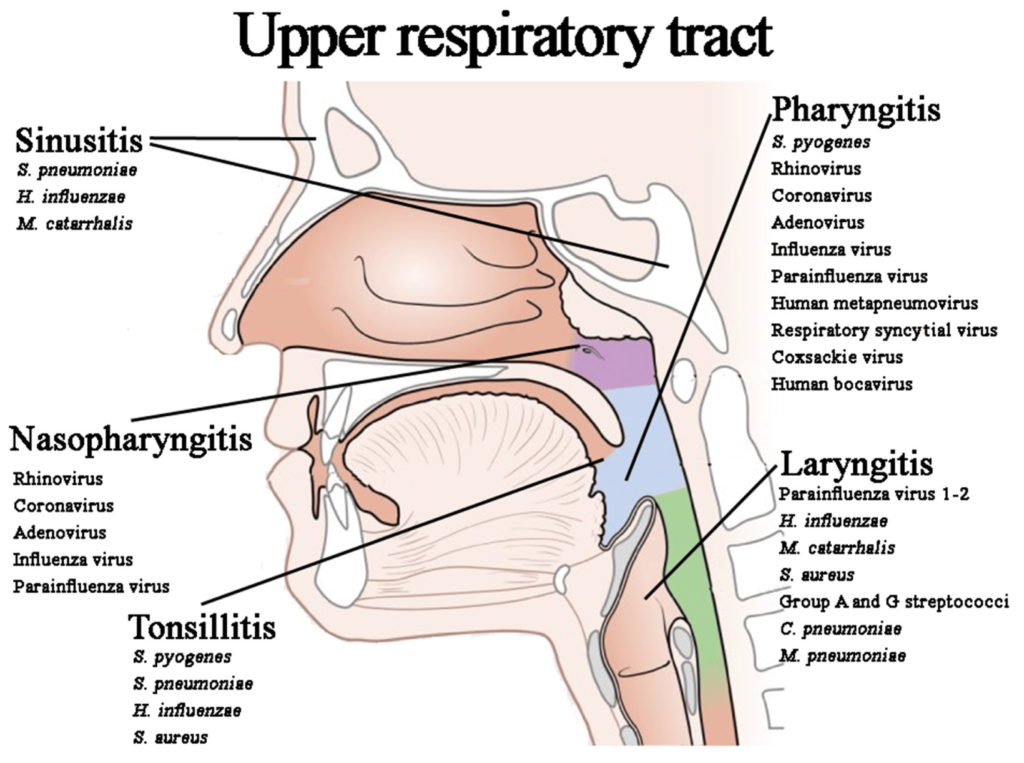
Pharyngitis

Pharyngitis, colloquially known as a sore throat, manifests as inflammation of the pharynx.
It manifests with various discomforts, including soreness, dryness, or scratchiness in the throat, accompanied by pain during swallowing or speaking. Additional symptoms may include fatigue, muscle aches, headaches, and fever. Viral infections such as the common cold, flu, or mononucleosis, bacterial infections like strep throat, and fungal infections in immunocompromised individuals are common culprits. Other factors contributing to pharyngitis may include allergies, muscle strain, and gastroesophageal reflux disease (GERD).
Diagnosis and Treatment
The diagnosis of pharyngitis involves a thorough physical examination along with laryngoscopy to pinpoint the underlying cause, whether viral, bacterial, or fungal. Treatment strategies vary accordingly. Viral pharyngitis typically resolves spontaneously with home remedies such as saltwater gargles, pain relievers, and adequate rest. Bacterial pharyngitis necessitates antibiotic therapy, whereas fungal pharyngitis is managed with antifungal medications. Timely administration of antibiotics is critical in cases of strep throat to prevent potential complications like kidney issues and rheumatic fever.
Prevention and Management
Preventive measures for pharyngitis entail maintaining proper hygiene practices, refraining from sharing food or utensils, regular handwashing, and avoiding smoking or exposure to secondhand smoke. While most instances of pharyngitis can be managed at home, seeking medical attention is imperative if symptoms persist beyond a week, if there’s a fever exceeding 100.4°F, swollen lymph nodes, a new rash, or if symptoms exacerbate following antibiotic treatment. Pharyngitis, though common, can be effectively addressed with appropriate care tailored to its underlying cause.
Tonsillitis

Inflammation and infection of the tonsils mark tonsillitis, a frequent ailment affecting those twin soft tissue structures nestled at the rear of the throat.Inflammation and infection of the tonsils mark tonsillitis, a frequent ailment affecting those twin soft tissue structures nestled at the rear of the throat. Serving as sentinels of the immune system, the tonsils intercept and apprehend harmful microbes that might incite infections.
During infection, these guardians swell, turn red, and become tender, causing discomfort like sore throats, fever, swollen lymph nodes, swallowing issues, and sometimes pale patches on tonsils.
Causes
Tonsillitis arises from either viral or bacterial origins. While viral causes predominate, bacterial culprits, notably Streptococcus bacteria, can also provoke this condition. Its contagious nature means it spreads easily through respiratory droplets or direct contact with those already afflicted. Factors that heighten susceptibility encompass youthfulness, frequent encounters with infectious pathogens, and weakened immune defenses.
Diagnosis and Treatment
A healthcare professional must conduct a thorough examination to detect tonsillitis, potentially involving a strep test to pinpoint bacterial involvement. Management strategies diverge depending on the root cause: viral instances call for rest and supportive care such as hydration and pain relief, whereas bacterial infections typically demand antibiotic intervention. For severe or recurring scenarios, the consideration of tonsil removal through surgical means (tonsillectomy) might be proposed as a viable course of action.
Prevention
Mitigating the onset of tonsillitis revolves around adhering to sound hygiene protocols, such as regular handwashing, steering clear of proximity to those harboring infections, and abstaining from the sharing of personal belongings. Early symptom spotting and rapid medical action assist in efficiently managing tonsillitis, preventing complications like peritonsillar abscesses.
Laryngotracheitis

Laryngotracheitis, commonly known as croup, manifests as inflammation affecting the larynx and trachea, often triggered by viral infections like the parainfluenza virus, particularly prevalent in children.
Common symptoms include a lingering cough, stridor (a high-pitched breathing sound), and hoarseness, often accompanied by fever. In infants, if inflammation spreads to the lower airways, laryngotracheitis can worsen, possibly causing complications.
Symptoms
Symptoms characteristic of laryngotracheitis, or croup, encompass a distinctive barky cough, hoarseness, stridor (manifesting as a high-pitched sound during breathing), and fever. In pediatric cases, this ailment may manifest with a cough, stridor, hoarseness, and fever. Progression to more severe forms might involve lower airway complications, marked by wheezing, crackles, reduced air movement, and rapid breathing (tachypnea). Patients exhibiting symptoms of laryngotracheitis can be stratified into mild, moderate, or severe categories based on their clinical presentation. Moreover, the identification of the “steeple sign” on chest X-rays, resulting from subglottic narrowing, serves as a hallmark feature aiding in croup diagnosis.
Management strategies
Management strategies for laryngotracheitis encompass a range of interventions drawn from the insights gleaned through research findings:
Utilization of Corticosteroids
Primary among these is the administration of corticosteroids, notably dexamethasone, which serves as a cornerstone in croup therapy. Oral steroid therapy, ranging from 0.15 mg/kg to 0.6 mg/kg, benefits all patients, not exceeding a one-time dose of 10 mg, regardless of severity.
Application of Nebulized Epinephrine
Another pivotal aspect involves the use of nebulized epinephrine to alleviate airway obstruction in croup sufferers. The recommendation extends to the utilization of racemic or L-epinephrine based on specified dosing guidelines.
Vigilant Monitoring
After each nebulized racemic epinephrine dose, it’s crucial to observe patients for at least 3 hours to spot any symptom worsening or recurrence.
Implementation of Humidified Air Therapy
For milder cases, the adoption of home-based moist air inhalation proves effective. Employing humidified oxygen or room humidifiers serves to forestall the exacerbation of inflammation caused by dry air.
Consideration of Hospitalization
Severe croup cases in infants and young children with hypoxemia, dehydration, or respiratory exhaustion may require hospitalization. High-risk groups like premature infants and children under 2 with bronchopulmonary dysplasia may need careful monitoring and hospitalization.
Potential Use of Intravenous Antibiotics
Tailored IV antibiotic therapy based on culture results may be necessary in suspected bacterial infections, especially in severe cases like epiglottitis.
Avoidance of Sedatives
Avoid sedatives that could depress respiratory drive in croup patients to reduce the risk of complications.
Summary
The article explores upper respiratory tract infections (URTIs), encompassing the nasal passages, sinuses, throat, larynx, and trachea. URTIs exhibit various symptoms like nasal congestion, sore throat, and fever, predominantly caused by viruses but also by bacteria, fungi, or helminths. Specific types of URTIs discussed include rhinitis, pharyngitis, tonsillitis, and laryngotracheitis, each with distinct causes and management strategies. Diagnosis involves a thorough examination, potentially including strep tests.
Treatment depends on the cause: viral infections often need rest and supportive care, while bacterial infections may need antibiotics. Prevention strategies emphasize proper hygiene and avoiding exposure to infectious agents. Treating severe cases like croup requires a comprehensive strategy with corticosteroids, nebulized epinephrine,and close monitoring. Possible hospitalization for high-risk patients. Overall, the article provides a comprehensive overview of URTIs, their causes, symptoms, diagnosis, treatment, and prevention measures.
Need more assistance click