Introduction
In the intricate web of human health, meningitis emerges as a formidable adversary that demands swift and decisive action. Persistent infections by stealthy bacteria can trigger inflammation of the protective membranes enveloping the brain and spinal cord, indicating a condition. The urgency of addressing meningitis lies in its potential to escalate swiftly, posing a serious threat to the central nervous system. Recognizing the telltale signs becomes paramount in this battle, where a spike in body temperature, throbbing headaches, unsettling dizziness, and the notorious stiffness of the neck serve as the first lines of defense against this silent intruder. As the body’s sentinel, it is imperative to decipher these signals promptly, unlocking the gates to timely treatment and safeguarding against the potentially grave consequences of meningitis.
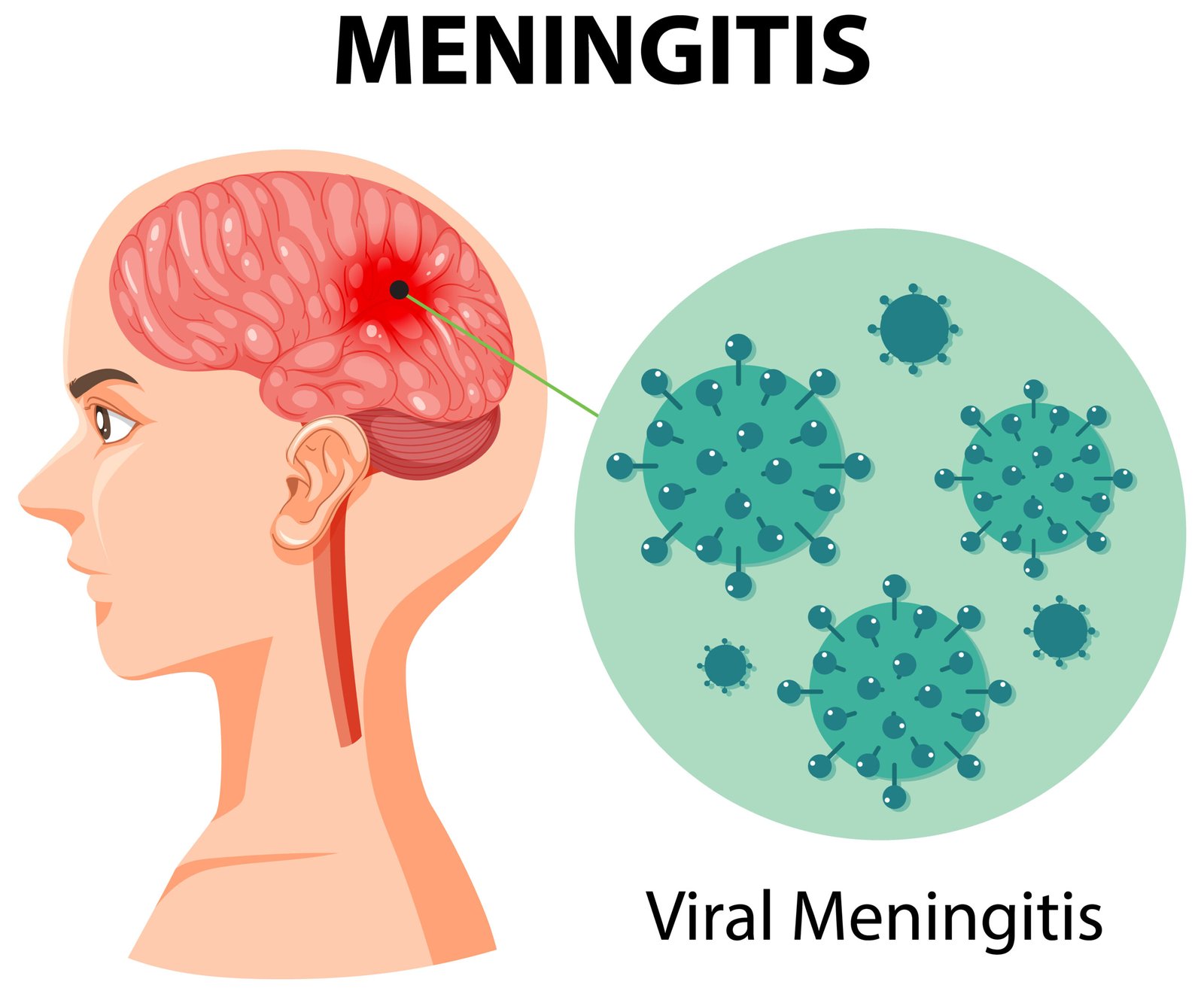
What is meningitis?

In the case of meningitis, also known as inflammation of the meninges of the brain or spinal cord, these are layers of connective tissue that cover the central nervous system. If the inflammation spreads directly to the brain, doctors speak of meningoencephalitis. Typically, a virus serves as the trigger, while less frequent yet considerably more perilous is bacterial-induced meningitis. Fungi, or parasites, can also be triggers.
Bacterial meningitis is sometimes also referred to as purulent meningitis, but it does not necessarily have to progress to a purulent state. The source lies in an infection by particular bacteria, such as pneumococci, Haemophilus influenzae, or meningococci. The latter poses a heightened risk, given its potential to cause a bloodstream infection (sepsis) with a high mortality rate. Fortunately, thanks in part to the availability of vaccines, cases of meningococcal disease are rare in Germany. Among the few cases, infants, young children, and adolescents are primarily affected. The immune system of infants and young children is still immature, providing little protection against infection. The protective vaccination against meningococci is recommended only at the age of twelve months. Adolescents, on the other hand, have a higher risk of infection due to their typically close and diverse social contacts.
Various viruses can also lead to the development of meningitis. Ticks widely recognize the tick-borne encephalitis virus (TBE virus) as one notable example, and they serve as vectors for transmitting these pathogens. Many other viruses are possible triggers, including the viruses that cause chickenpox or mumps. The herpes simplex virus and the Epstein-Barr virus (which can lead to infectious mononucleosis), as well as Coxsackie viruses (among others, the causative agents of hand, foot, and mouth disease), can also be the cause of meningitis. Droplet infection typically transmits them.
Must Read: Urinary Tract Infections (UTIs): Clinical Practice Guideline
Symptoms: How does meningitis manifest itself?
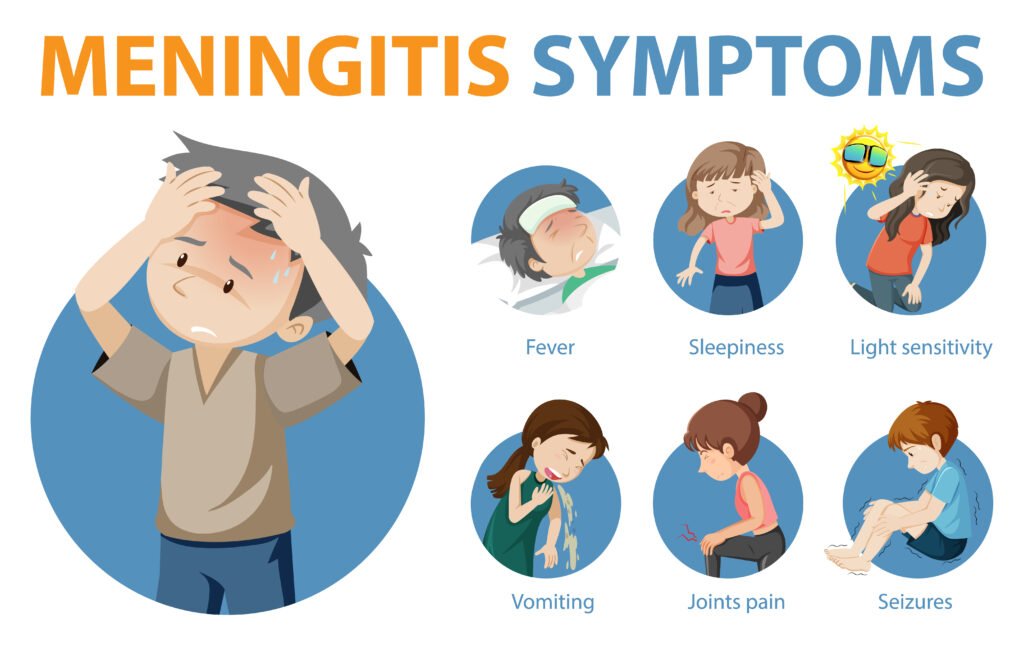
The first signs of meningitis are usually severe headaches, a high fever, and fatigue. A characteristic is neck stiffness, which may be absent in infants.
It arises from inflammation in the membranes of the brain and spinal cord, commonly known as meningism. Bending the head towards the chest is hardly possible due to inflammation-induced pain. Often, nausea, vomiting, and high sensitivity to noise and light (photophobia) also occur. Confusion, seizures, and disturbances of consciousness, up to unconsciousness, are also possible. If infected with meningococci, tiny dot-like spots may emerge on the skin due to bleeding.
Emergency ! A meningococcal disease can become life-threatening within a few hours and is therefore always an emergency. Meningococcal disease can manifest as meningitis, occasionally also as a bloodstream infection (sepsis), and must be treated as quickly as possible. If you suspect meningococcal disease, call the emergency medical service or an emergency doctor. Meningococcal diseases are treated in the hospital on an inpatient basis, as they almost always have a severe course and frequently lead to complications.
What is the treatment for meningitis?
A medical examination of the cerebrospinal fluid in the spinal canal, also known as brain or nerve fluid, can identify the pathogens causing meningitis. The treating physician conducts this analysis by performing a lumbar puncture and inserting a hollow needle into the lumbar vertebrae area to extract a small amount of fluid from the spinal canal. Certain blood values, including white blood cells and a differential blood count, C-reactive protein, and the erythrocyte sedimentation rate, also provide indications of inflammation in the body.Sometimes, healthcare providers may use imaging procedures, for instance, when it becomes necessary to exclude other potential causes of the symptoms.
Furthermore, healthcare providers may recommend preventive antibiotic treatment for close contacts such as family members, daycare attendees, or schoolmates.
For viral meningitis, healthcare providers primarily treat the symptoms by ensuring adequate fluid intake and administering pain relievers, fever-reducing medications, and anti-nausea drugs.
Can you protect yourself against meningitis through vaccination?

The Permanent Vaccination Commission (STIKO) at the Robert Koch Institute (RKI) recommends including vaccinations against meningococcal type C, pneumococci, and Haemophilus influenzae type B as part of the essential immunization for children. These provide protection against infections or severe forms of diseases caused by these pathogens. In doing so, the vaccinations also significantly reduce the risk of bacterial meningitis.
Health authorities advise vaccinating all children against meningococcal C at the age of twelve months, and it is important to catch up on any missed vaccinations before the 18th birthday. Basic immunization against pneumococci and Haemophilus influenzae type B is recommended starting at two months of age.
The STIKO recommends incorporating vaccinations for children into the basic immunization program to protect against viral diseases such as chickenpox, measles, mumps, rubella, and poliomyelitis, which could be associated with meningitis or meningoencephalitis.
The STIKO recommends vaccination for individuals in exposed groups against tick-borne encephalitis (TBE), a viral disease prevalent in the region.
Meningitis NHS
Meningitis, a potentially life-threatening condition, is a topic of paramount importance within the realm of the National Health Service (NHS). The NHS plays a crucial role in its prevention, diagnosis, and treatment. Inflammation of the protective membranes surrounding the brain and spinal cord characterizes it. The NHS, as a cornerstone of public health in the United Kingdom, strives to raise awareness about the symptoms of meningitis, emphasizing the significance of early detection. Through vaccination programs, public health campaigns, and accessible healthcare services, the NHS endeavors to safeguard the population against this formidable infectious threat.
The organization’s commitment to research and education ensures that it equips healthcare professionals with the latest information on meningitis. Contributing to a comprehensive approach to tackling this challenging medical condition. Healthcare providers and the NHS collaboratively continue to fight the battle against meningitis on multiple fronts. Emphasizing the paramount importance of proactive healthcare initiatives in the face of potential public health crises.
Summary
Inflammation of the protective membranes surrounding the brain and spinal cord characterizes meningitis, a serious medical condition. It may result from different factors, such as viruses, bacteria, fungi, or parasites. The urgency of addressing meningitis lies in its potential to escalate quickly into a serious threat to the CNS.
The symptoms of meningitis include severe headaches, high fever, fatigue, neck stiffness, nausea, vomiting, and photophobia (sensitivity to light). In the case of meningococcal disease, tiny dot-like spots on the skin result from bleeding.
Considering meningococcal disease a medical emergency is crucial, as it can turn life-threatening within a few hours. Treatment involves hospitalization and the prompt administration of antibiotics. For some viruses, doctors may recommend antiviral therapy while primarily treating symptoms in the case of viral meningitis.
Health authorities recommend including these vaccines as part of the essential immunization program for children. It’s crucial to recognize the early signs of meningitis to facilitate timely treatment and prevent potential complications.