Escherichia coli (E. coli) are gram-negative, mostly motile rod bacteria from the family Enterobacteriaceae. They are undemanding and grow both aerobically (with oxygen) and anaerobically (in the absence of oxygen). As non-pathogenic commensals, Escherichia coli are an obligatory component of the colon flora of most warm-blooded mammals, many birds, and humans.
There are also so-called pathovars that have pathogenicity factors and can trigger diseases. Such pathogenicity factors are primarily adhesion mechanisms that mediate attachment to host cells and the formation of toxins that intervene as poisons in the metabolic processes of the host cell or destroy host cells
Disease-Causing Agents and their Mode of Spread
- Certain E. coli strains produce a cell toxin called Shiga toxin or Vero toxin. This interchangeably leads to the terms verotoxin-producing (VTEC) and shigatoxin-producing E. coli (STEC).
- EHEC, short for enterohemorrhagic Escherichia coli, refers to certain strains of the intestinal bacterium Escherichia coli. These strains have additional pathogenic factors and can cause severe inflammatory reactions in humans.
- The primary cause of VTEC infections often stems from the consumption of specific untreated animal products, such as inadequately cooked minced beef and unpasteurized milk.
- Contaminated foods like yogurt, salami, cheese, raw veggies, and unpasteurized apple juice are sources of outbreaks.
- Infections can result from improper slaughter, animal contact in petting zoos, cow-dung-fertilized meadows, or person-to-person transmission.
In most cases, the illness is self-limiting, but it may lead to a life-threatening disease, including hemolytic uraemic syndrome (HUS), especially in young children and the elderly.
Medical Presentation
- The incubation period for the infection ranges from one to eight days.
- Numerous VTEC infections manifest without evident symptoms, often eluding detection.
The illness typically begins with watery diarrhea, evolving into a mix of watery and bloody stools as it progresses.- Concurrent symptoms encompass nausea, escalating abdominal pain, occasional fever, and vomiting.
- Historical data suggests severe illnesses are more common in infants, children, the elderly, and immunocompromised individuals.
- In severe cases, toxins may cause anemia, harm organs, and lead to kidney failure, known as HUS.
- The mortality rate from HUS is notably elevated among children.
Read also: Chickenpox Chronicles: Navigating a Varicella-Infected World
E. Coli Infection: Recognizing the Symptoms
Escherichia coli, commonly known as E. coli, is a bacterium that resides in the intestines of humans and animals. While most strains of E. coli are harmless, certain varieties can cause infections with unpleasant symptoms. Recognizing the signs of an E. coli infection is crucial for prompt medical attention and effective treatment.
Common Symptoms
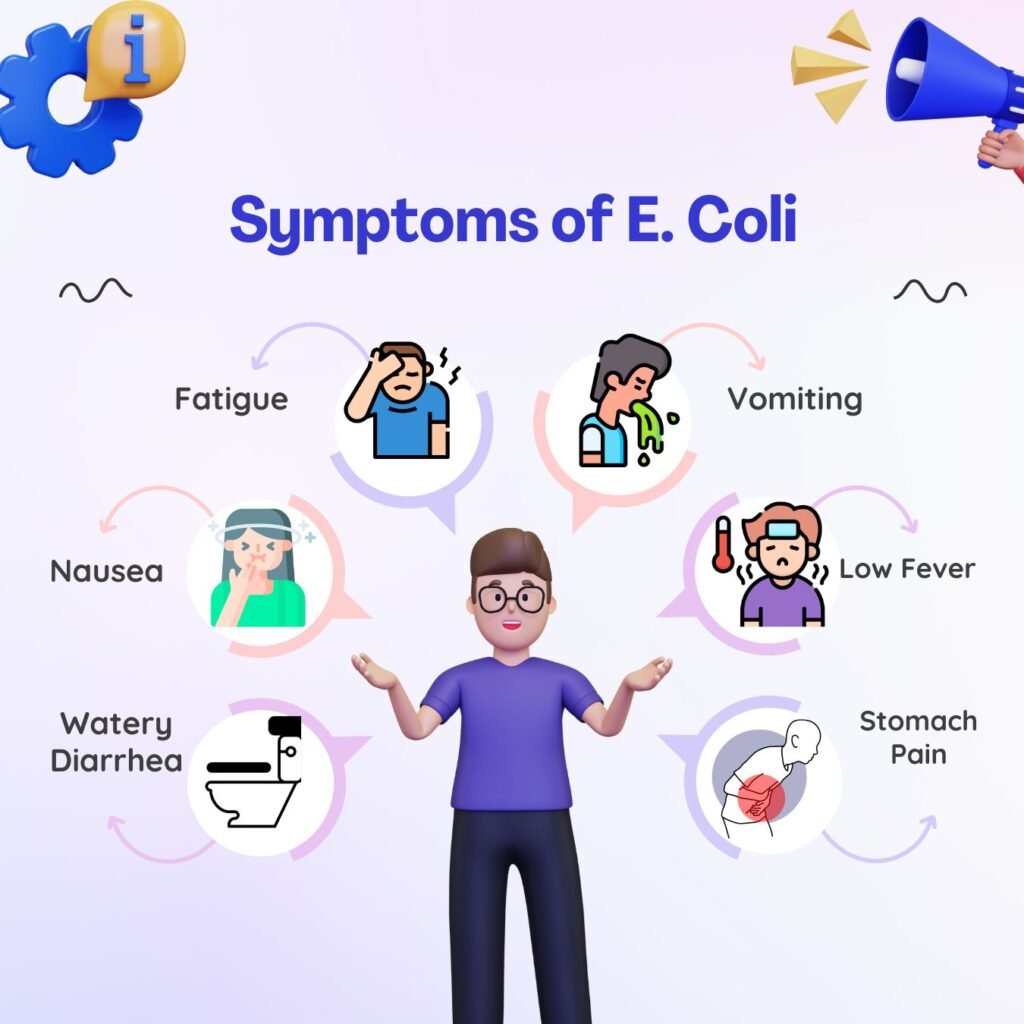
1. Gastrointestinal Distress
One of the primary indicators of an E. coli infection is gastrointestinal distress. This can manifest as severe abdominal cramps, stomach pain, and tenderness. Individuals may also experience nausea and vomiting, contributing to the overall discomfort.
2. Diarrhea
E. coli infections often lead to diarrhea, which can range from mild to severe. The diarrhea may be bloody, accompanied by an urgency to use the restroom. Dehydration is a concern in more severe cases, necessitating immediate medical intervention.
3. Fever
A noticeable increase in body temperature is another symptom of an E. coli infection. Fever is the body’s response to the presence of harmful bacteria, signaling an immune system response. Monitoring and managing fever are essential components of addressing an E. coli infection.
Less Common Symptoms
1. Hemolytic Uremic Syndrome (HUS)
In rare cases, E. coli infections can lead to a severe condition known as hemolytic uremic syndrome (HUS). This syndrome is characterized by kidney failure, anemia, and a low platelet count. Symptoms may include decreased urination, fatigue, and unexplained bruising.
2. Urinary Tract Infections (UTIs)
E. coli can also cause urinary tract infections, leading to symptoms such as frequent urination, pain or discomfort during urination, and cloudy or foul-smelling urine. UTIs require specific medical attention and treatment.
3. Neonatal Meningitis
Neonatal meningitis caused by E. coli is a serious and potentially life-threatening infection affecting newborns, highlighting the importance of early detection and prompt medical intervention.
When to Seek Medical Attention
1. Persistent Symptoms
If symptoms persist or worsen over time, it is essential to seek medical attention promptly. Persistent diarrhea, especially if accompanied by blood or mucus, should not be ignored.
2. Signs of Dehydration
Dehydration is a significant concern with E. coli infections. Symptoms include dark urine, reduced urine output, dry mouth, and lethargy. Immediate medical care is crucial to prevent complications associated with dehydration.
Diagnosing E. Coli: A Guide

Escherichia coli (E. coli) is a bacterium that can cause various infections in humans, ranging from mild gastrointestinal discomfort to severe complications. A timely and accurate diagnosis is crucial for effective management and treatment. This guide provides insights into the methods and procedures used in diagnosing E. coli infections.
Clinical Assessment
1. Symptom Evaluation
The first step in diagnosing an E. coli infection involves a thorough assessment of the patient’s symptoms. Gastrointestinal distress, including abdominal pain, cramps, vomiting, and diarrhea, is commonly observed. Notably, the presence of bloody or persistent diarrhea may raise suspicion.
2. Medical History
A detailed medical history helps healthcare professionals identify potential sources of E. coli exposure. Questions about recent travel, food consumption, and contact with infected individuals are essential for narrowing down the diagnostic possibilities.
Laboratory Tests
1. Stool Culture
Stool cultures are a primary diagnostic tool for E. coli infections. A small sample of the patient’s stool is collected and cultured in a laboratory to identify the specific strain of E. coli responsible for the infection. This test also helps determine the presence of antibiotic resistance.
2. PCR Testing
Polymerase Chain Reaction (PCR) testing is a molecular technique used to detect the genetic material of E. coli. PCR is highly sensitive and can provide rapid results, aiding in the swift diagnosis of infections.
Additional Diagnostic Measures
1. Blood Tests
In severe cases or when complications are suspected, blood tests may be conducted to assess the overall health of the patient. Elevated white blood cell counts and signs of systemic infection can indicate the severity of the E. coli infection.
2. Imaging Studies
In certain situations, imaging studies such as abdominal X-rays or CT scans may be recommended to assess the extent of complications, especially if there are concerns about conditions like hemolytic uremic syndrome (HUS).
E. coli: Disease Avoidance
The primary safeguard involves maintaining personal and kitchen hygiene, with an emphasis on consistent handwashing. No vaccines or preventive medications are available. To minimize infection risks, adhere to the following guidelines:
- Refrigerate raw animal-derived and perishable foods (e.g., meat, Mettwurst, cold cuts, milk, milk products, and delicatessen salads).
- Thoroughly wash raw vegetables before consumption.
- Store raw foods separately.
- Clean work surfaces, tools, and hands diligently after handling raw food.
- Ensure thorough cooking, particularly of meat, with a core temperature of at least 70 °C for 10 minutes.
- After interacting with animals, especially ruminants (e.g., petting zoos or farms), cleanse hands meticulously with warm water and soap, drying them using disposable paper towels.
- Consume food and beverages away from areas with animal contact.
E. coli Bacteremia
E. coli bacteremia, a condition arising from the presence of Escherichia coli bacteria in the bloodstream, represents a serious medical concern. This bloodstream infection can result from various sources, such as urinary tract infections, gastrointestinal issues, or other underlying health conditions. E. coli, a normally harmless inhabitant of the human intestines, can become pathogenic when it enters the bloodstream, leading to symptoms like fever, chills, and a general feeling of malaise. Prompt and appropriate medical intervention is crucial to managing E. coli bacteremia effectively, often involving targeted antibiotic therapy. As microbial resistance patterns evolve, ongoing research aims to enhance our understanding of this condition and refine treatment approaches, highlighting the importance of a comprehensive and dynamic approach to managing bacterial infections.
Summary
This article explores Escherichia coli, a bacterium present harmlessly in human, mammal, and bird intestines. It delves into harmful strains causing severe illnesses, such as Vero toxin-producing Escherichia coli (VTEC) and enterohemorrhagic E. coli (EHEC), discussing adhesion mechanisms and toxin production.
The text examines disease transmission sources, including untreated animal products and person-to-person spread. VTEC infections are detailed, emphasizing the potential severity, particularly hemolytic uraemic syndrome (HUS), in vulnerable populations.
Recognizing E. coli infection symptoms, like gastrointestinal distress and diarrhea, is crucial. The article mentions less common symptoms, such as urinary tract infections and neonatal meningitis.
The third section covers diagnosis methods, including clinical assessment, medical history, stool culture, PCR testing, blood tests, and imaging studies.
The conclusion stresses disease avoidance through personal and kitchen hygiene. Despite the absence of vaccines, adherence to guidelines like refrigeration, vegetable washing, and thorough cooking is vital.
The final part highlights E. coli bacteremia’s seriousness, necessitating prompt medical intervention with targeted antibiotic therapy. Ongoing research is crucial to understand and address evolving microbial resistance patterns.